Hundreds of thousands of women world-wide use menstrual tracking apps to predict fertile days and to prevent pregnancy. These apps are great for tracking the monthly cycle and have provided valuable data for understanding menstrual cycles in real-world women. But they are not great at predicting fertile days. Most menstrual apps identify fertile days based on traditional assumptions about the female hormonal cycle leading many women to miss their fertile window. The main assumption being that a ‘normal’ or ‘average’ cycle is 28 days long with little variation and ovulation occurring consistently on day 14.
Historic assumptions on cycle length, follicular phase length, ovulation and luteal phase length are outdated and wrong yet most apps continue to develop programs based on this misinformation.
One recent study from Mount Sinai Hospital in Toronto warned that 1 in 5 menstrual apps have errors that could affect chances of pregnancy. Although this seems like big news, Time Magazine reported on similar findings back in 2016. Most fertility experts have been aware of this issue for years yet many women remain unaware that using apps to get pregnant can be misleading. I have seen this in practice with a number of women experiencing difficulty getting pregnant who are using cycle tracking apps. Once we identify the correct fertile window, they are able to conceive.
Cycle Length in Real Women, Real Cycles.
A 2019 study (1) that utilized data from fertility tracking apps analyzed 612,613 ovulatory cycles from 124,648 users. This is one of the largest sample sizes ever collected! The average follicular phase length was 16.9 days with a variance of 10-30 days while the average luteal phase length was 12.4 days with variance of 7-17 days. The average cycle length decreases by 0.18 days per year and the average follicular phase length decreases an average of 0.19 days per year in women between the ages of 25 to 45 years. Mean variation of cycle length per woman was 0.4 days or 14% higher in overweight women compared to women with a normal body mass index.
The data from this study and from other studies suggests that the female menstrual cycle has much more variability than assumed. In the above study only 13% of menstrual cycles were 28 days long while less than 1% of cycles were longer than 50 days. Overall, 91% of women had cycles between 21-35 days long.
Interestingly, very short cycles had shorter bleed lengths and very long cycles had longer bleed length. The very short cycles had shorter follicular phase by 5.4 days and shorter luteal phases by 4.4 days. The very long cycles had longer follicular phase by 11.0 days and longer luteal phases by 0.6 days.
Yet another study showed that a woman who experiences variations of less than 8 days between her longest and shortest cycle is considered normal. Irregular cycles are generally defined as having 8 to 20 days variation in length of cycle, whereas over 21 days variation in total cycle length is considered very irregular (4).
This is a lot of variability! The individual woman needs more information on her unique cycle to accurately pinpoint fertile days and identify ovulation. To understand what information is useful, we need to understand the phases of the menstrual cycle.
The Follicular Phase (The First Half of the Cycle)
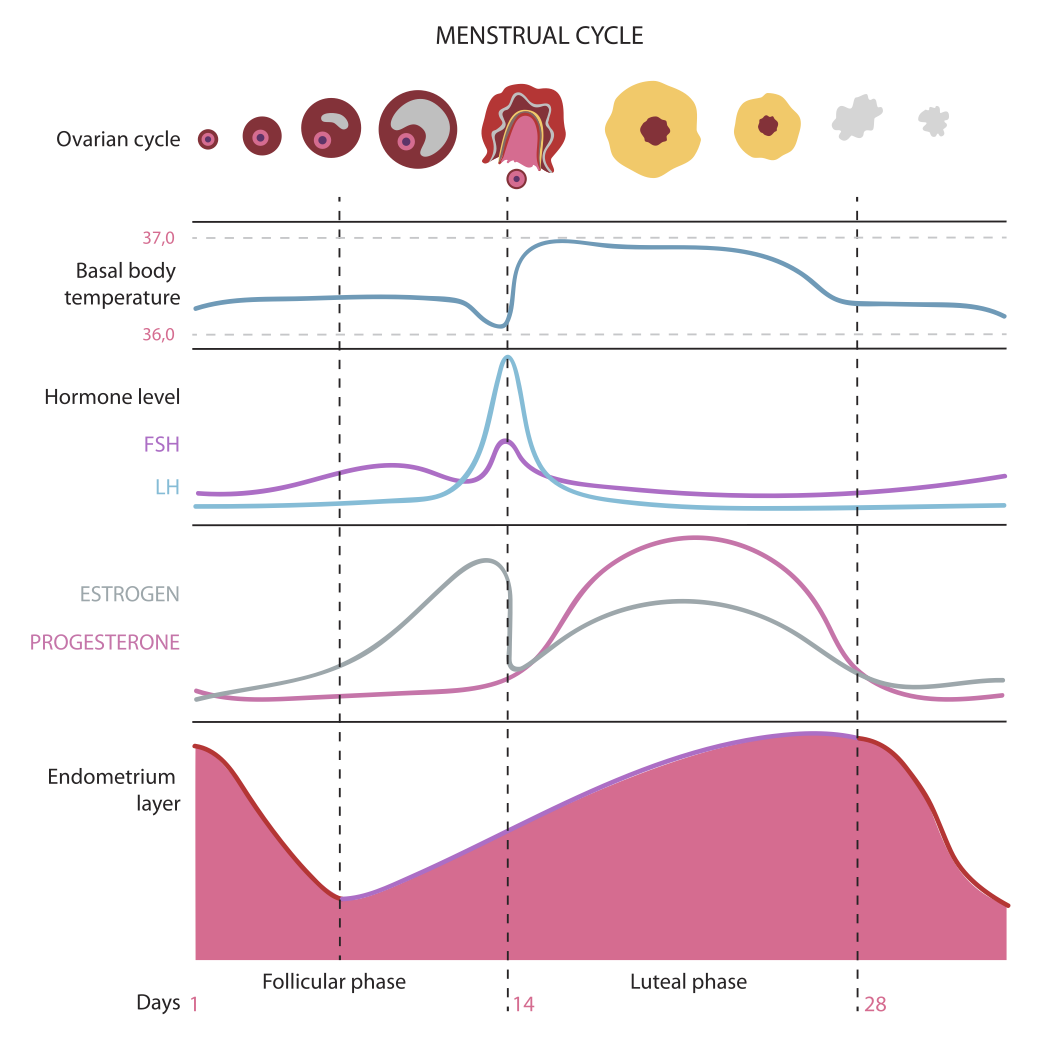
The follicular phase begins on the first day of menstruation and continues until ovulation. Lower body temperatures and the development of ovarian follicles characterize this phase.
When there is variability in a woman’s menstrual cycle length, most of this variability occurs in the follicular phase which is more vulnerable to physical, emotional, nutritional and environmental changes. As discussed above, follicular phase length appears to be on average, 16.9 days with a variance of 10-30 days. If you went based on this finding, you would only predict an accurate ovulation date 13% of the time! Yet another reason why a standard ‘day 14 assumption’ for ovulation doesn’t make sense.
The follicular phase of the cycle is considered estrogen dominant. Estrogen levels rise and fall twice during the menstrual cycle. Estrogen levels rise during the mid-follicular phase and then drop sharply after ovulation. Rising levels of estrogen produced by the growing ovarian follicle cause another hormone, lutenizing hormone (LH) to rise (2).
Causes of Follicular Phase Variations
There are a number of factors that influence the follicular phase and can make cycle tracking tricky. Certain foods, substances, medications, environmental changes, exercise, weight loss and stressors can all affect cycle length and the follicular phase seems to be the most vulnerable. For example, occasional marijuana users (up to 3 times in the last 3 months) had a longer follicular phase than non-users (3.5 days); frequent users (>3) were almost two days longer than non-users. Meanwhile, Vitamin D deficiency has been shown to cause a longer follicular phase (6). These are just two examples of cycle influencers. There are many more! Understanding why your follicular phase changes may require a lifestyle and diet assessment by an experienced practitioner.
Ovulation (Release of Fertile Egg)
Ovulation occurs approximately 10-12 hours after the LH peak which occurs in the follicular phase. The beginning of the LH surge occurs roughly 34 to 36 hours (some studies suggest 28-48 hours) prior to ovulation and is a relatively precise predictor for timing ovulation (1,3). The spike in LH causes the mature ovarian follicle to rupture, releasing an egg.
Interesting Fact! In humans, ovulation probably occurs randomly from either ovary during any given cycle. Of interest, some studies have suggested that ovulation occurs more commonly from the right ovary and right sided ovulation carries a higher potential for pregnancy
The Luteal Phase (The Second Half of the Cycle)
After the follicle ruptures and the egg is released, a structure called the corpus luteum forms on the ovary, marking the start of the luteal phase. This phase lasts up until menstruation begins. The corpus luteum secretes progesterone for the duration of the luteal phase in order to get the uterine lining (the endometrium) ready for embryo implantation. During this time, the uterine lining grows thicker as the body prepares for possible pregnancy. It is considered a progesterone dominant part of the menstrual cycle although there is a secondary spike in estrogen that parallels the increase in progesterone at this time. Due to the levels of progesterone, there is a distinct rise in body temperature of 0.2–0.3 °C following ovulation. This rise in body temperature continues if pregnancy occurs.
In the late luteal phase, progesterone starts to drop which causes a reduced blood supply to the uterus. This eventually leads the uterus to contract and slough off layers of the endometrium, AKA menstruation.
Many healthcare providers still believe that the luteal phase is consistently 14 days in length and that any cycle variability originates from the follicular phase. However, studies have shown that there is some variability in the luteal phase (12.4 days ± 2.4 days) albeit considerably less than in the follicular phase. This means that if a woman wanted to take a shortcut with her app, she would be better off to count 14 days backwards from the last day of her cycle to arrive at a more likely day of ovulation (most apps count forward from the first day of menstruation). Yet she may still be inaccurate. A more complete tracking system is recommended!
Tracking the Fertile Window: A Complete Fertility Tracking System
The fertile window, during which there is a likelihood of conception, is defined as the day of ovulation and the 5 days preceding it. Sperm can live up to 5 days in the vagina and female reproductive tract and so pregnancy can result from unprotected sex on any of the 5 days before ovulation.
A Complete Tracking System involves diligent tracking of Basal Body Temperature (BBT), Cervical Mucus and LH urine strips.
Basal Body Temperature
Basal body temperature (BBT) is defined as the ‘lowest natural, non-pathologic body temperature recorded after a period of rest’. BBT measurements have been used to help women understand their fertile window. Tracking BBT will typically reveal a noticeable increase of approximately 0.5 to 1 degrees F shortly after ovulation. Body temperature increases and then sustains until it drops shortly before menstruation.
The ‘thermal nadir’ (the lowest point of body temperature), occurs 1-2 days after the LH surge, approximately 1 day preceding the onset of ovulation (3). For most accurate results, temperatures need to be recorded at the same time every day, immediately upon waking up (while still in bed). Measurements are affected by environmental factors such as fever/illness, emotional stressors, alcohol consumption, and the addition or discontinuation of oral contraception; BBT results are inaccurate when these factors are present.
The fertile window will typically be in the 3-4 days prior and 1 day after to the ‘thermal nadir’ or lowest body temperature seen before a sustained spike. Tracking BBT tends to be accurate for women with a ‘normal cycle length’ (21-35 days) but it isn’t perfect (3) and is best used with the other tracking tools discussed below.
Interesting Fact! There are new technologies (vaginal biosensors) that measures core temperature every 5 min and represent an evolution in the accuracy of the determining the window of fertility (5).
Cervical Mucus
Immediately after menstruation, the cervical mucous is scant and viscous. During the late follicular phase, under the influence of rising estrogen levels, the cervical mucous becomes clear, copious and elastic. The quantity of cervical mucous increases 30x compared to the early follicular phase. After ovulation, as progesterone levels rise, the cervical mucous once again becomes thick, viscous and opaque and the quantity produced by the endocervical cells decreases (2).
Identifying when cervical mucous is clear, copious and elastic to when it becomes thick, viscous and opaque can help to identify ovulation. In plain terms, a woman can track stringy/clear vs sticky/white cervical mucous. Analyzed alongside BBT, these details help to identify ovulation and the 5 day fertile window.
LH Urine Strips
LH urine strip tests kits are available at most drug stores and can help you pinpoint when the LH hormone starts to rise, allowing you to be more precise with ovulation. The beginning of the LH surge occurs roughly 34 to 36 hours before ovulation while the LH peak occurs 12 hours before ovulation. You will see an elevation in LH from the urine strips on only 2-3 days of your cycle. Your fertile window will be approximately 3 days before you start to see LH rise and up to ½ a day past the LH spike.
Although LH strips are great indicators, they are best used in combination with other indicators such as BBT and cervical mucous to properly track the full window of 5 days. Also, there is no need to use LH strips on every day of your cycle. On average, using the strips from Day 10 of your cycle to Day 21 will typically catch the LH surge. If you don’t catch a surge after attempting a couple months, it may be time to seek out some professional advice.
Steps to Follow:
Find yourself a physical or virtual Fertility Tracking Calendar. I am a fan of the chart from Baby Centre. Physical charts are easy to use, and the patterns can be easier to see.
Start Tracking! Repeat for 3 months to get a good amount of cycle data.
If you find you are experiencing trouble with tracking or are getting confusing results, it can help to visit a practitioner who focuses on fertility tracking. It may be that lifestyle or dietary changes are affecting your results or it may be that you need further hormonal work-up.
Summary:
Many of the assumptions made in menstrual apps that track fertility are wrong. The majority of women don’t ovulate on day 14 of their menstrual cycle and attempting to get pregnant in the 5 days fertility window around day 14 can lead to difficulties with conception. What is now known to be ‘normal’ is not a 28 day cycle. Rather, most women have cycles between 21-35 days. It is also normal for a woman to have a changing cycle length up to 8 days. When the cycle length changes, it is the follicular phase (typically) that has changed although recent research has shown that the luteal phase may also vary. Therefore, every women needs to track her own unique cycle over a period of time (I recommend 3 months minimum!) or it is quite likely that they will miss their chance to conceive. This means tracking a combination of BBT, cervical mucous and LH spikes to determine the 5 day window of fertility.
References
1. Bull JR, Rowland SP, Scherwitzl EB, Scherwitzl R, Danielsson KG, Harper J. Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ Digit Med. 2019;2:83. Published 2019 Aug 27. doi:10.1038/s41746-019-0152-7
2. Reed BG, Carr BR. The Normal Menstrual Cycle and the Control of Ovulation. 2018 Aug 5. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279054/
3. Steward K, Raja A. Physiology, Ovulation, Basal Body Temperature. [Updated 2019 Aug 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan
4. Fehring RJ, Schneider M, Raviele K. Variability in the phases of the menstrual cycle. J Obstet Gynecol Neonatal Nurs. 2006 May-Jun;35(3):376-84. PubMed PMID:16700687.
5. Regidor PA, Kaczmarczyk M, Schiweck E, Goeckenjan-Festag M, Alexander H.Identification and prediction of the fertile window with a new web-based medical device using a vaginal biosensor for measuring the circadian and circamensual core body temperature. Gynecol Endocrinol. 2018 Mar;34(3):256-260.
6. Jukic AM, Weinberg CR, Baird DD, Wilcox AJ. Lifestyle and reproductive factors associated with follicular phase length. J Womens Health (Larchmt). 2007;16(9):1340–1347. doi:10.1089/jwh.2007.0354